How Effective Is Large Vessel Occlusion (LVO) Treatment in Improving Stroke Outcomes?
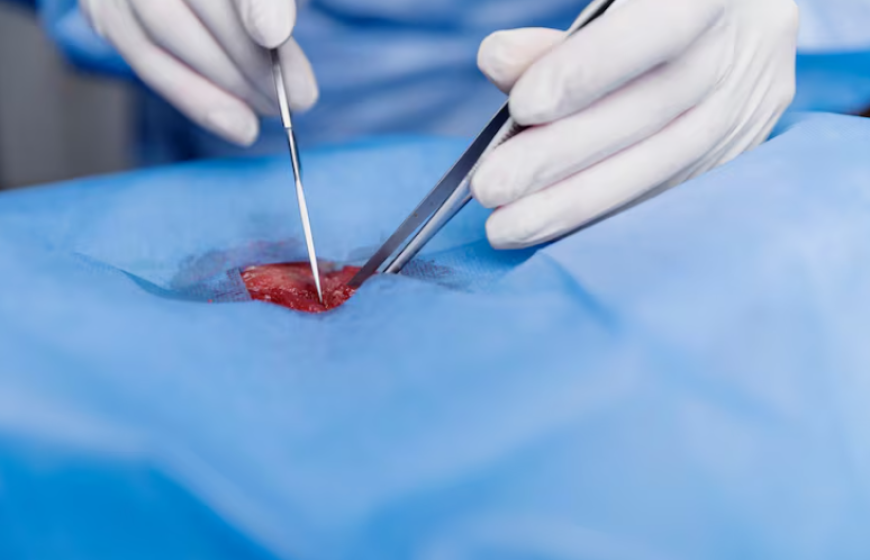
LVO, or Large Vessel Occlusion, is a blockage of major cerebral arteries that causes severe ischemic stroke. For eligible patients, standard care is endovascular therapy. This method removes clots using stent retrievers or aspiration systems. Many high-quality trials show that thrombectomy greatly lowers disability. This is true when patients are carefully chosen compared to just using medical management.
Evidence: functional outcomes and expanded indications
Recent randomized trials and meta-analyses prove that early thrombectomy yields lasting benefits. Early studies showed big gains at 90 days. Newer trials, like SELECT2 and ANGEL-ASPECT, reveal that a larger group, once seen as unlikely to improve, is now benefiting. This evidence supports treating more patients. It considers hemorrhage risk and each patient's imaging results.
Who benefits most?
Patients with large vessel occlusions (LVO) in the anterior circulation get the best results when treated on time. Those with favorable imaging show higher rates of independence, lower disability, and reduced mortality. The First-Pass Effect, achieving complete or near-complete reperfusion on the first attempt, results in significantly better outcomes and fewer complications, which makes procedural efficiency a critical quality metric.
Routine thrombectomy for low-NIHSS LVOs and some distal or medium-vessel occlusions should be tailored to each case. More evidence is needed before making standard guidelines.
Real-world caveats and post-acute care
Swift triage, precise imaging, skilled operators, and rigorous post-thrombectomy rehabilitation protocols guarantee effectiveness. The data show that some subgroups, like those with very mild strokes, gain little benefit and may have higher sICH risks. This highlights the need for multidisciplinary case selection and standardized rehab protocols to promote better recovery through reperfusion.
Simulation, training, and improving outcomes
Operator skills improve with better training, team drills, and device use. This leads to higher First-Pass Effect rates and faster reperfusion times. Angio-compatible simulators empower teams to master real workflows through direct, hands-on practice.
Surgeonslab's thrombectomy simulator offers realistic endovascular scenarios. It helps clinicians master aspiration and stent strategies. They can also refine balloon-guide techniques and improve first-pass outcomes. This translates directly to improved patient results.
Bottom Line
Mechanical thrombectomy for Large Vessel Occlusion Treatment gives great results for carefully selected patients. This makes it a top choice for acute intervention in modern medicine. It helps prevent disabilities from strokes. Surgeonslab's realistic simulators empower doctors with targeted training, maximizing these benefits.
